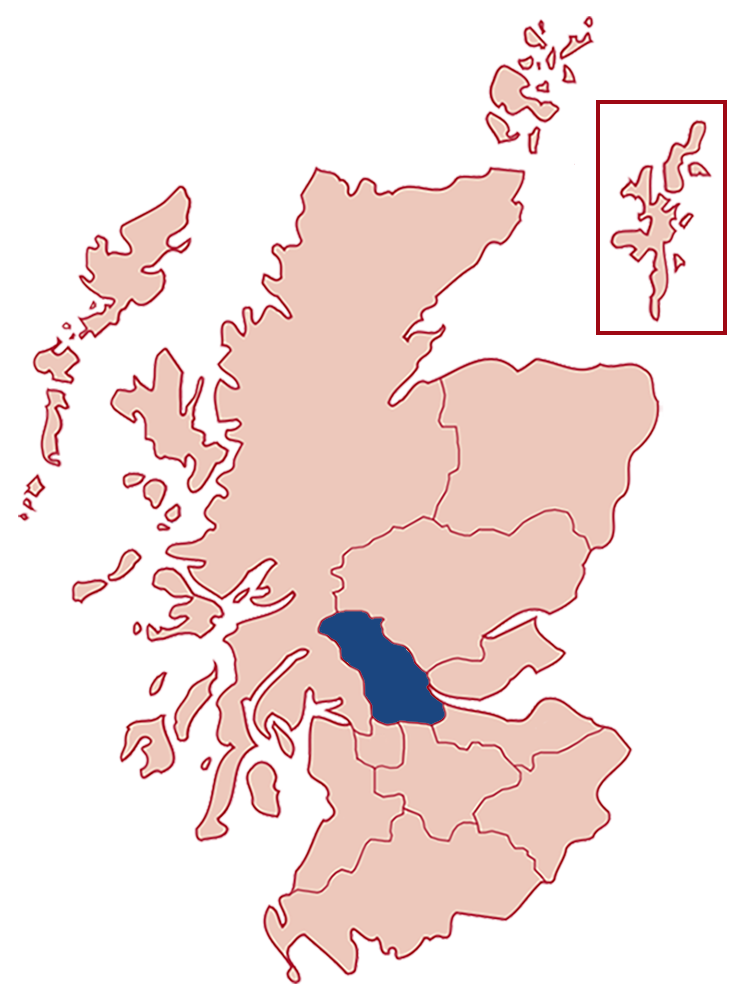
Forth Valley
Patients per year
480
from 300 in 2012.
Urban / rural split
75%
from 80% in 2012.
Total region population
305,000
from 293,386 in 2012.
Specialist HF nurse WTE posts
3.35 WTE (5 staff)
from 3 WTE, from 4 staff in 2012.
Service provision
| 2012 | 2018 |
|---|---|
| HFrEF | HFrEF |
| HFpEF | HFpEF |
| HF post MI | HF post MI |
| Valvular HF | Valvular HF |
| Congenital HF | Congenital HF |
| Palliative Care | General palliative care and 1 HF specialised palliative care nurse - direct links to specialist care |
| Cardiac Rehabilitation for HF | |
| Screening for psychological distress- no direct referrals to psychology |
Service model
| 2012 | 2018 |
|---|---|
| Home | Home |
| Clinic | Clinic |
| In-pt education | In-pt education |
| In-pt management | In-pt management |
| GP surgery | GP surgery |
| Virtual | Virtual |
Additional notes
Service achievements
- Implemented Heart failure MDT
- Day case diuretic in Cardiology Day Unit, Participating in Heart Failure research
- Smooth introduction for assessment of suitability for Entresto, device and arrhythmia MDT.
- Increased use of and protocol for Subcutaneous Furosemide in the community
- Access to Natriuretic peptide testing
Service challenges
- Improved access to psychology service (when escalation required
Future improvements
- To speed up the process of diagnosis of outpatients following Natriuretic peptide testing by GP with same day echo and review of patients with elevated Natriuretic peptide.
- To undertake a scoping exercise with for HFpEF/Right sided HF patients.
- To scope options for a heart failure inpatient unit.
REMINDER
The following details are from our 2012 report and may not reflect the current state of the Forth Valley Health Board.
Further details
| (Actual number of staff) | 2008 - 3.2 WTE (4 staff) |
| SIGN Ratio | 1:97,795 (2008 1:89,392) |
| Ave. caseload per post | 140 (community and hospital) |
| Individual patients managed by service (average year) | 300 patients |
| Service Provision | Home visits 20% / Clinic Appointments 80% |
| Provision for HF-PEF | No |
| Administration support per week | 30 hours (across service) |
| Providing education to non-specialist staff | Yes – Secondary care: individual and group teaching with staff nurses and healthcare assistants in cardiology wards and clinics; Primary care: create meetings |
| Doctor with specialist interest in Heart Failure | Yes - 1 Consultant |
| Cardiac Rehabilitation available/number seen | Yes - 50 patients per year |
| Access to psychological support referral pathway | Adequate |
Notes on current service provision
Manage patients with LVSD and symptomatic Heart Failure. Referrals received from wards, Cardiology and other clinics, Open Access Echocardiography and General Practice. Actively discharge patients once optimised and stable; liaise with SNAHFS as appropriate.
Funding in comparison to 2008
Core funded by NHS Forth Valley
Challenges
Only one nurse undertakes outreach visits for Forth Valley. Managing in-patient workload with out-patient clinics and unpredictability of help-line calls all stretches service provision. Increasingly complex patients, particularly those with significant renal dysfunction. Unable to respond to demand to review patients with HF-PEF.
Development opportunities
HF nurses, in conjunction with consultants, implement evidence- based medicine in patients admitted with decompensation using the HF bundle and a holistic approach incorporating discharge planning. Access to Day Medicine Unit for patients who require IV diuretics. Provide pre-op assessment and education for patients undergoing implantation of a cardio-defibrillator [ICD].