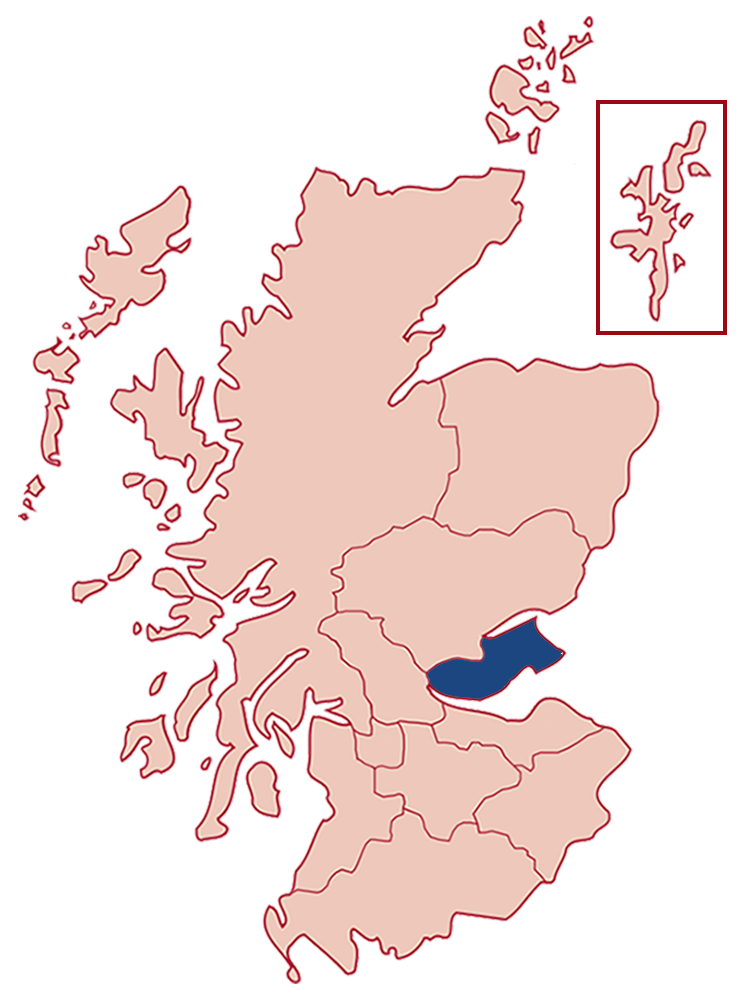
Fife
Patients per year
287
from 238 in 2012.
Urban / rural split
82%
from 79% in 2012.
Total region population
368,808
from 364,945 in 2012.
Specialist HF nurse WTE posts
2 WTE (2 staff)
from 2 WTE, from 2 staff in 2012.
Service provision
| 2012 | 2018 |
|---|---|
| HFrEF | HFrEF |
| HFpEF | HFpEF |
| HF post MI | HF post MI |
| Valvular HF | Valvular HF (only with LVSD) |
| Congenital HF | Congenital HF |
| Palliative Care | General palliative care with links to specialist services |
| Cardiac Rehabilitation for HF | |
| Screening for psychological distress- no direct referrals to services |
Service model
| 2012 | 2018 |
|---|---|
| Home | Home |
| Clinic | Clinic |
| In-pt education | In-pt education |
| In-pt management | In-pt management |
| GP surgery | GP surgery |
| Virtual | Virtual |
Additional notes
Service achievements
- Development of HF support group.
- Redesign of community cardiac services
Service challenges
- Staffing levels to meet demand
Future improvements
- Redesign of community cardiac services
REMINDER
The following details are from our 2012 report and may not reflect the current state of the Fife Health Board.
Further details
| (Actual number of staff) | 2008 * 2 WTE (2 staff) |
| SIGN Ratio | 1:182,473 (2008 1:179,429) |
| Ave. caseload per post | 70 (community) |
| Individual patients managed by service (average year) | 238 patients |
| Service Provision | Home visits 80% / Clinic Appointments 20% |
| Provision for HF-PEF | Yes – cardiologist referral with management plan in place |
| Administration support per week | 9 hours (across service) |
| Providing education to non-specialist staff | Yes – 1 hour sessions to GP surgeries raising awareness of service pathway and refresher on heart failure management |
| Doctor with specialist interest in Heart Failure | 1 Consultant Cardiologist (specialist interest) |
| Cardiac Rehabilitation available/number seen | Limited - no referral pathway |
| Access to psychological support referral pathway | Inadequate (waiting list of up to 6 months) |
Notes on current service provision
In 2010, the service moved from management by the Acute Operating Division to within Primary Care. Service redesign is ongoing to ensure that the service is being utilised to maximum effect. An increase in telephone consultations and developing locality clinics allows us to continue to see patients close to their homes and cuts down time and money (mileage) spent travelling to home visits. By developing closer working relationships and sharing the more stable caseload with the vascular teams in the CHPs, the service can see more patients. A lot of work has been carried out to develop and implement the heart failure care bundle, with MCN support.
Funding in comparison to 2008
Core funded by NHS Fife.
Challenges
Despite increasing demand, we are able to keep a manageable caseload by transferring the care of more stable patients to the vascular services in the CHPs. Our case load number does not reflect the true amount of referrals coming into and being discharged from the service.
Development opportunities
We are opening referrals to other types of heart failure e.g. HF-PEF and inoperable valve problems (if referred by a cardiologist with a management plan). Widening the criteria has not overwhelmed the service and input from the service has reduced hospital admissions and improved the patient’s quality of life. We are participating in a 2 year Telehealth pilot and a multidisciplinary heart failure clinic for both new and existing referrals.